What is a Dexa Scan?
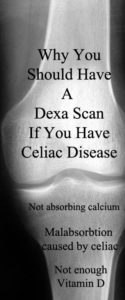
Dexa or DXA is actually an acronym for Dual X-ray Absorptiometry. While it is a type of x-ray it isn’t quite the same as an x-ray. Your bone density would have to be severe in order to see it on an x-ray. The radiation from the Dexa Scan is much lower than other x-rays and scans.

A Dexa Scan measures how thick and strong your bones are AKA bone density. The test is rated on a T-score. The higher your T-score the better. If you have a low T-score, your chances of breaking bones are greater. Our bones are the strongest at age 30 and so your results will be compared to someone with really good bones at age 30.
A doctor can order tests to be on a Z-score. Which is where your results are compared to someone who is your age and body size.
The test only takes about 20 minutes. This test is for Osteopenia or Osteoporosis. (Osteopenia is early Osteoporosis.)
What are Osteopenia and Osteoporosis?
Osteopenia– means your bones are losing their density and becoming more spongy instead of thick and strong. This means you are more likely to break a bone than the average person your age and bone size.
Osteoporosis– is severe bone loss. This puts you at risk for many fractures because your bones are becoming brittle.
Why do I need a Dexa Scan? Isn’t this test for old women?
Dexa Scans are typically used for older women in their 60s. So, why would someone (male or female) with celiac need a Dexa Scan?
Osteoporosis isn’t just a woman’s disease! It affects millions of men too! Celiac causes malabsorption which can lead to not absorbing enough Vitamin D and calcium causing brittle bones. It is a complication of celiac disease and not necessarily gender specific.
Here are more factors that can cause lower bone density
- Celiac disease (especially undiagnosed, undiagnosed for many years, and/or poor adherence to the gluten free diet)
- inflammation (http://celiacblog.mayoclinic.org/2014/08/22/bone-density-and-celia-disease/)
- Heredity- family members who have osteoporosis
- Being underweight- as well as those who are petite and slender (have a greater risk)
- Amenorrhea- sporadic periods, early menopause (before 45 years old) and or estrogen deficiency
- Having an inactive (sedentary) life style
- Excessive Exercise
- Extreme dieting and/or eating disorders
- Smoking
- Alcohol use- can interfere with absorption of calcium and vitamin D
- Caffeine
- Other diseases: thyroid disease, diabetes, food allergies, Crohn’s, Multiple Sclerosis, to name a few.
- Treatments and mediations can lead to osteoporosis
- Stress
- Low vitamin D
- Too much sodium
- Poor nutrition or poor absorption
Risk Factors For Men
All of the above plus:
- Long term use of medications: steroids from asthma meds, arthritis meds., anti-convulsants, and cancer treatments (not a complete list)
- Hormone levels- low testosterone
Warning signs typical in men
- loss of height
- change in posture
- fracture
- sudden back pain
The Celiac Connection to Osteoporosis
From an article in Gluten Free Living:
“In the general population, osteoporosis strikes patients most often when they’re in their 50s and 60s. But in patients with celiac disease, you can see osteoporosis 15 years earlier,” says Donald Kirby, MD, director for the Center for Human Nutrition at the Cleveland Clinic in Cleveland. Osteoporosis can often set in over the age of 65, but for untreated celiac disease patients the bone disease can even occur in childhood.
People with celiac have a higher risk for osteoporosis compared to the general population. Also, those with celiac are more likely to develop the disease at a younger age.
The good news is that with adherence to the gluten free diet those with celiac can regain their bone mass! *This may not be completely true for all with celiac; some may still have a reduced bone mass compared to others in their age and body group. Additional supplements may be needed. Also important is to know what your Vitamin D levels are and to work with your doctor to get the right amount of Vitamin D for your body.
*I am not a doctor. I am offering suggestions on a direction to research, as wells as, what I have learned from my experiences. Please, always do your own research and consult your doctor about your health choices.
The Importance of Vitamin D
Did you know that you can’t absorb calcium properly if you are Vitamin D deficient? It is important to get the proper amount of Vitamin D and calcium. This will help your bones!
Consult your doctor for help in getting proper nutrition. A good doctor to consult about vitamins and minerals is a medical internist. Most likely you need more than a good multi-vitamin. (Make sure to check all supplements for gluten! Many supplements contain gluten and because they are not a food product it does not have to be listed on the label!)
Why you should have a base-line Dexa Scan
Bone density is used as a surrogate marker for fractures. Studies that have compared celiac disease patients with healthy controls have shown celiac disease patients at diagnosis have lower bone densities at the hip and spine. Similar studies have also shown bone density correlates with damage at the gastrointestinal level. This means the more malabsorption, the lower the bone density. Pulling the reports together, 50-70% of patients with celiac disease will have some type of low bone density.
(http://celiacblog.mayoclinic.org/2014/08/22/bone-density-and-celia-disease/)
Many people don’t know they have Osteopenia or Osteoporosis until they have a fracture. Considering that 50-70% of patients with celiac disease have low bone density it is a good idea to know where you are, so you can make adjustments and take precautions.
It is also good to have a point of reference. If you wait for years before getting one done, you won’t know if you have improved or gotten worse.
My Experience
I had my first Dexa-Scan when I was 35 years old. I was one of the lucky ones. I don’t know what my score was, but I didn’t have Osteopenia or Osteoporosis.
I had another one when I was 38, at the same place. The technician was actually looking at both while I was in the room. She told me it looked great and had actually improved since last time! Then she said I wasn’t bad last time, but looked even better now!
It’s time to have another one! It has been 10 years and I’m way overdue for one! However, with my recent gravity check I don’t think I have anything to worry about!
My Husband’s Experience
 My husband had a Dexa-Scan years ago when he was first diagnosed with non-celiac gluten intolerance. They said he had osteopenia. He was hesitant about the medication and after a friend had some severe side-effects from some osteoporosis meds he researched and decided he didn’t want to take them.
My husband had a Dexa-Scan years ago when he was first diagnosed with non-celiac gluten intolerance. They said he had osteopenia. He was hesitant about the medication and after a friend had some severe side-effects from some osteoporosis meds he researched and decided he didn’t want to take them.
About a year later, we were roller skating and my husband fell. He broke his ankle in 3 places and had a spiral fracture in his calf. There were so many brakes because of the skates and the way he fell. The doctor said he didn’t have osteopenia or he would have broken a lot more; like his wrist and hip that came down so hard!
We were also told that studies aren’t very comprehensive on men; especially young men. (Younger than 65 years) Though he does have some of the above risk factors: always been thin, pretty sedentary, lots of gastro issues.
The most recent test
Not sure what my husband has; he can’t be officially diagnosed with Crohn’s because he doesn’t have any scar tissue; though he has the other things seen with Crohn’s. The doctor believes the lack of scar tissue may be due to removing his biggest trigger for Crohn’s which would be gluten! So, while he isn’t able to get a clear diagnosis, his gluten free diet has saved him from a lot of pain and other problems!
With all of this in mind the doctor wanted to check and see where things were at with his bones. It’s been 10 years since the last Dexa-Scan. He just went this morning and so we don’t have any results.
He also went to a different facility than he had before and this facility has the dexa scan in the “Women’s Imaging”. Seems very short sighted considering this disease isn’t just a woman’s disease!!!
He sat in a waiting room of women, most of whom were waiting to have mammograms; he was incredibly uncomfortable!
Improving Bone Density
- If you have celiac disease be strict on your gluten free diet!
- Exercise, but not excessively
- Take a good multi-vitamin (make sure all vitamins and supplements are gluten free)
- Take Vitamin D and possibly calcium (consult your doctor have your vitamin levels checked)
- Lower inflammation (I take Turmeric, but there are a lot of diet suggestions online for lowering inflammation)
- Have hormone levels checked
- Stop drinking alcohol and caffeinated drinks
- Stay hydrated- Drink plenty of water
- Stop smoking
- Eat less sodium
- Talk to your doctor about help with medications and treatments that may be contributing to bone loss
- Discuss with your doctor when to have repeat Dexa Scans- many with osteoporosis do them yearly, others every 3-5 years.
- Do your own research! Can diet alone help your symptoms? What are the risks of osteoporosis medications and are there other things that would help?
*I am not a doctor. I am offering suggestions on a direction to research as wells as what I have learned from my experiences. Please always do your own research and consult your doctor about your health choices.
Resources where I found Information
https://www.niams.nih.gov/Health_Info/Bone/Osteoporosis/men.asp
http://www.osteopenia3.com/Cause-of-Osteopenia.html
http://www.webmd.com/osteoporosis/guide/dexa-scan
http://www.osteopenia3.com/Dehydration-Osteopenia-Osteoporosis.htm






7 Comments
Leave your reply.